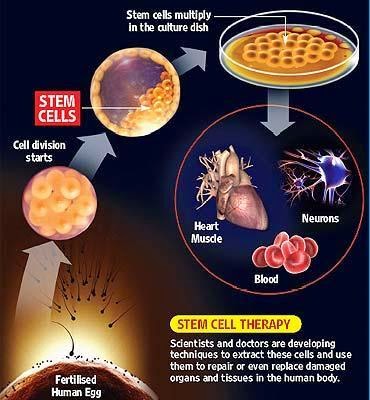
A statistical model has been created that measures the
proportion of cancer incidence, across many tissue types, caused mainly by
random mutations that occur when stem cells divide. By this measure, two-thirds
of adult cancer incidence across tissues can be explained primarily by “bad
luck,” when these random mutations occur in genes that can drive cancer growth,
while the remaining third are due to environmental factors and inherited genes.
Scientists
from the Johns Hopkins Kimmel Cancer Center have created a statistical model
that measures the proportion of cancer incidence, across many tissue types,
caused mainly by random mutations that occur when stem cells divide. By their
measure, two-thirds of adult cancer incidence across tissues can be explained
primarily by "bad luck," when these random mutations occur in genes
that can drive cancer growth, while the remaining third are due to
environmental factors and inherited genes.
"All cancers are caused by a combination of bad
luck, the environment and heredity, and we've created a model that may help
quantify how much of these three factors contribute to cancer development.
"Cancer-free longevity in people exposed to
cancer-causing agents, such as tobacco, is often attributed to their 'good
genes,' but the truth is that most of them simply had good luck," adds
Vogelstein, who cautions that poor lifestyles can add to the bad luck factor in
the development of cancer.
 |
| Figure 1: 3D DNA model |
 |
| Figure 2: Random DNA
Mutation |
Researchers claim 65%
of cancer cases are a result of random DNA mutations, while the remaining 35%
can be explained by a combination of these mutations and environmental and
hereditary factors. The implications of their model range from altering public
perception about cancer risk factors to the funding of cancer research, they
say. "If two-thirds of cancer incidence across tissues is explained by
random DNA mutations that occur when stem cells divide, then changing our
lifestyle and habits will be a huge help in preventing certain cancers, but
this may not be as effective for a variety of others," says bio-mathematician Cristian Tomasetti, Ph.D., an assistant professor
of oncology at the Johns Hopkins University School of Medicine and Bloomberg
School of Public Health. "We should focus more resources on finding ways
to detect such cancers at early, curable stages," he adds.
To sort out the role of such random mutations in cancer
risk, the Johns Hopkins scientists charted the number of stem cell divisions in
31 tissues and compared these rates with the lifetime risks of cancer in the
same tissues among Americans. From this so-called data scatterplot, Tomasetti
and Vogelstein determined the correlation between the total number of stem cell
divisions and cancer risk to be 0.804. Mathematically, the closer this value is
to one, the more stem cell divisions and cancer risk are correlated.
"Our study shows, in general, that a change in the
number of stem cell divisions in a tissue type is highly correlated with a
change in the incidence of cancer in that same tissue," says Vogelstein.
One example, he says, is in colon tissue, which undergoes four times more stem
cell divisions than small intestine tissue in humans. Likewise, colon cancer is
much more prevalent than small intestinal cancer.
"You could argue that the colon is exposed to more
environmental factors than the small intestine, which increases the potential
rate of acquired mutations," says Tomasetti. However, the scientists saw
the opposite finding in mouse colons, which had a lower number of stem cell
divisions than in their small intestines, and, in mice, cancer incidence is
lower in the colon than in the small intestine. They say this supports the key
role of the total number of stem cell divisions in the development of cancer.
Using statistical theory, the pair calculated how much of the variation in
cancer risk can be explained by the number of stem cell divisions, which is
0.804 squared, or, in percentage form, approximately 65 percent.
Finally, the research duo classified the types of cancers
they studied into two groups. They statistically calculated which cancer types
had an incidence predicted by the number of stem cell divisions and which had
higher incidence. They found that 22 cancer types could be largely explained by
the "bad luck" factor of random DNA mutations during cell division.
The other nine cancer types had incidents higher than predicted by "bad
luck" and were presumably due to a combination of bad luck plus environmental
or inherited factors.
"We found that the types of cancer that had higher
risk than predicted by the number of stem cell divisions were precisely the
ones you'd expect, including lung cancer, which is linked to smoking, skin
cancer, linked to sun exposure, and forms of cancers associated with hereditary
syndromes," says Vogelstein.
"This study shows that you can add to your risk of
getting cancers by smoking or other poor lifestyle factors. However, many forms
of cancer are due largely to the bad luck of acquiring a mutation in a cancer
driver gene regardless of lifestyle and heredity factors. The best way to
eradicate these cancers will be through early detection, when they are still
curable by surgery," adds Vogelstein.